How much are vaccinations worth? Here in north-central Idaho, common killed virus shots for spring branding total nearly $4 per cow and just under $8 per calf from the local vet. With that kind of investment, proper handling has to be a priority for producers.
“We want to maintain the integrity of the vaccine itself so it will do its job,” says K. Scott Jensen, University of Idaho (UI) extension educator in Owyhee County. He adds that, ultimately, the reason for caring about vaccine integrity is the same reason for administering vaccinations at all: “to keep our animals healthy.”
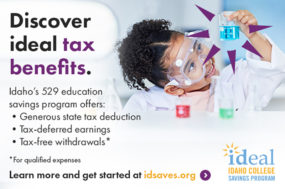
However, a 2009-10 UI case study indicated that only 33% of producers’ vaccine-storing refrigerators maintained the recommended temperature range (35ºF to 45ºF) more than 95% of the time, and 33% of refrigerators were within that range less than 5% of the time.
“I’d heard and read about [proper vaccine storage],” says Mike Kossler, a now-retired Lemhi County rancher who participated in the study, “but I never gave it much thought that I should check my own fridge.”
An Idaho producer case study
The results from the UI study were similar to those gathered in Nevada and Arkansas around the same time. Jensen had read about these studies in The Professional Animal Scientist and sought funding from the Idaho Beef Council to investigate how Idaho compared.
Lemhi County Extension Educator Shannon Williams joined Jensen in recruiting volunteers and executing the study. “We had temperature trackers – LogTags – that we put in producers’ refrigerators where they were storing vaccines,” she says. These data loggers recorded the temperature every 10 minutes for at least 48 hours. Once compiled, the data revealed that a vast majority of producers surveyed were storing vaccine at temperatures outside manufacturers’ specifications (Figure 1).
For many, the solution was as simple as adjusting the refrigerator’s temperature controls. This was particularly true for those in garages or outbuildings when the outside temperature reached extremes.
Others ended up buying new refrigerators entirely. Not Bruce Mulkey – another Lemhi County rancher who participated in the study – though. He laughs, “I kind of wanted a new refrigerator, but ours was one of the better ones, so we kept it.” However, he now keeps a temperature monitor in that old refrigerator.
Regardless of refrigerator type or age, researchers recommend using a thermometer and storing vaccine on the middle shelves for most consistent temperatures.
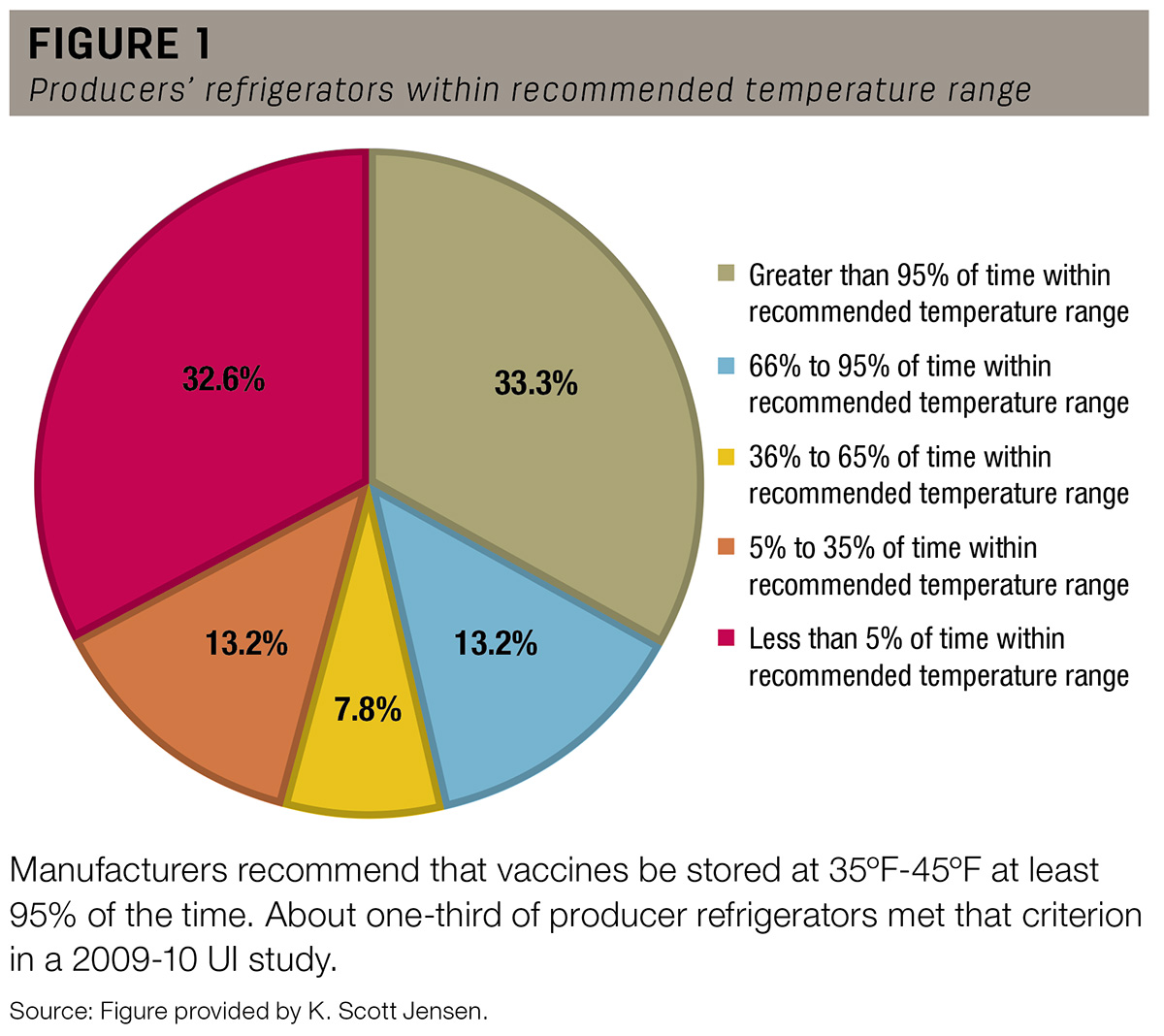
 Researchers recommend that producers purchase vaccine from a reputable source, discard after open or expired and store unopened bottles on the middle shelves of a temperature-monitored refrigerator. Photo by Julia McCarthy.
Researchers recommend that producers purchase vaccine from a reputable source, discard after open or expired and store unopened bottles on the middle shelves of a temperature-monitored refrigerator. Photo by Julia McCarthy.
The vaccine middle man
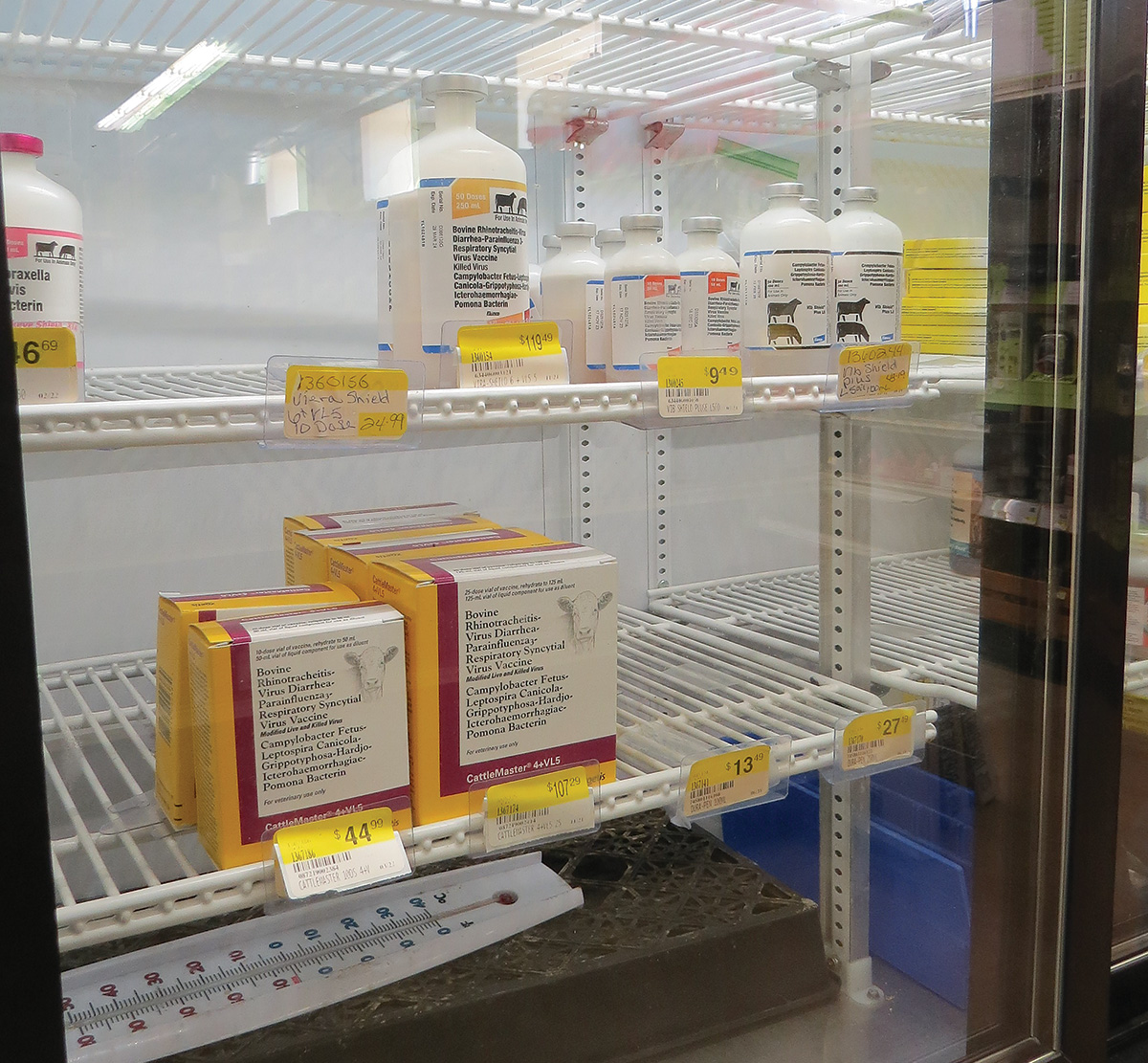
Some retail outlets also participated in the study. “It started out as a side project,” says Jensen. “It didn’t look good, but we didn’t have the numbers, so we went back and added in more retailers.”
Similar to producers, only 34% of the surveyed retailers’ refrigerators maintained an appropriate temperature at least 95% of the time (Figure 2).
This concerned researchers. Even the best vaccine handling strategies cannot make up for product that has already been compromised before purchase. “When you go to wherever you buy vaccines, ask, ‘Do you have a thermometer in there?’ and ‘How often is it checked?’” advises Jensen.
Alternately, Williams says, “If you mail order, make sure you order on Monday so the vaccine isn’t sitting over the weekend. Then, as soon as you get it, open the package and make sure it is cold.”
How much fluctuation is too much?
It’s an interesting study, but you may ask: What’s the big deal? One consideration is that vaccine manufacturers will not stand behind product stored outside the temperature range on the label.
As for maintaining vaccine effectiveness: “On one side, it’s pretty nebulous,” says Jensen. “We don’t know how fast vaccine efficacy declines when it’s too warm.” That probably depends on the vaccine, the adjuvants, the temperature and other factors.
On the other hand, Jensen calls a frozen vaccine “immediately worthless” because ice crystals change the structure of the adjuvant. “The recommendation on any vaccine that freezes for any period of time – whether it’s three seconds or an hour – is to throw it out immediately,” he says.
Other storage considerations
Another component of the study involved inventorying producers’ medicine refrigerators. Of the 2,257 bottles found in 129 refrigerators, 21% were expired and 27% had been opened. These open bottles included both killed and modified-live virus (MLV) vaccines. Jensen recommends disposing of MLV vaccines within an hour of mixing and killed virus vaccines within 10 days of opening.
A killed virus vaccine does not break down as speedily as an MLV, but it can host contamination. “When you open a bottle, you’re introducing bacteria, no matter how clean you try to be,” Jensen explains. “Those bacteria then multiply, even in a fridge.”
Researchers also noted whether vaccine was stored in a refrigerator with food or drink for human consumption. Besides concerns about temperature fluctuation with frequent door opening, bottles that have been handled at the chute can introduce bacteria into a refrigerator.
Vaccines in action
For both Kossler and Mulkey, the most interesting aspect of the project involved chuteside protocol. “We became more careful, especially at the corral,” says Kossler of his family’s practices after the study. “It woke me up there. I think we were doing OK before, but it made me pay more attention.” Kossler went so far as to drill holes into Styrofoam coolers to store multiple-use syringes in between applications.
The biggest change on the Mulkey ranch was the type of cooler used at a branding. “We always followed BQA protocol anyway,” Mulkey says. However, they discontinued use of soft-sided coolers after Williams borrowed one and learned how much faster it heated up than firmer alternatives. “I know [the hard-sided cooler] keeps it cold,” he says.
The researchers recommend following BQA protocol and offer common-sense advice. “If you’re close to the house, refill the cooler after your lunch break,” says Williams. “Only bring out as much vaccine as you need.”
The researchers followed up the study by providing individualized recommendations to each producer and retailer who participated. “We tried to be educational,” Jensen says.
Ultimately, most of those participants were appreciative. “Vaccine is expensive,” Kossler says. “If it’s not working right, then you’re just going through the motions.”